| |
Circumcision and Pain

|
Contents
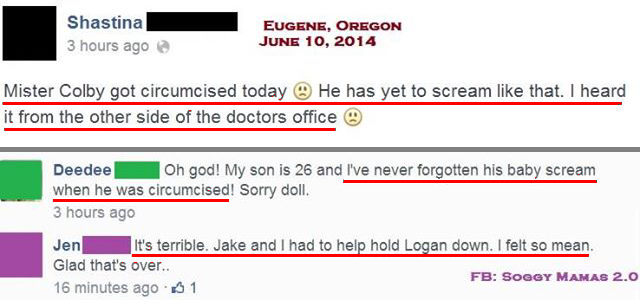
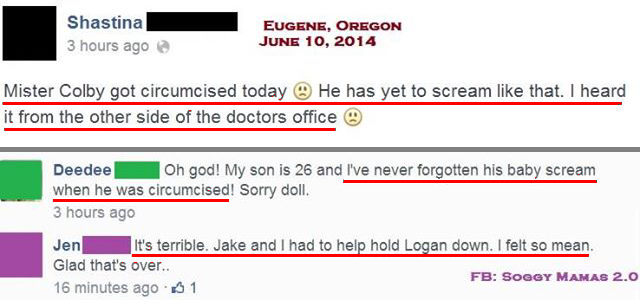
Anecdotes
Studies
Babies feel pain...
...more than adults ...
... even with anaesthetic ...
...(sugar is no good)...
And the pain may resume after the circumcision is
over. "It was nothing like his cries when he got his
shots. Nothing like when he came out of the womb.
Nothing like anything he'd done yet. It was a deep
cry - totally from pain. It was evident through his
entire body." Blog of a
father whose baby had extreme post-operative pain.
... and it has long-term effects.
Other
|
|
Dr S lays Sarah's baby on the bench. "You're not
going to faint, are you?" he asks me. "That's the
main injury risk round here." He straps Bobby to a
rack, known as a Circumstraint. Bobby rails a little
as Dr S swabs his pubis with Betadine. "This will
hurt a bit," says the doctor, injecting anaesthetic
into the base of the penis.
Bobby spits his dummy and starts wailing
while Dr S loosely ties a silk thread around the
tiny penile shaft. The foreskin is attached to the
glans and has to be forcibly freed before it is
clamped, stretched and slit. This widens the
aperture to accommodate the "Plastibell", basically
a notched thimble which fits over the head of the
penis.
Bobby's wails are getting louder,
and Dr S looks slightly uncomfortable. "They don't
all cry like this," he says. He manoeuvres the
thread over the Plastibell notch and gives a sharp,
hard tug. The crying stops.
Bobby's limbs go rigid, his eyes bulge, his mouth
gapes and his fingers snap straight. Then his body
goes limp and all is quiet.
Dr S
looks mildly dismayed. "About one in two jump like
that." He waits a few minutes before slicing off the
strangled foreskin and breaking off the Plastibell
handle. "The ring will fall off in about five days.
Really, it's no more risky or difficult than doing
sheep's tails." With that, he buttons Bobby into his
babysuit. The entire operation has taken eight
minutes.
"How
was he?" Sarah asks the doctor when we return to the
waiting room. "Fine," he says. "Give him a feed and
he'll be right."
- from "Losing It" by John van Tiggelen
the Sydney Morning Herald / The Age (Melbourne)
26 August, 2000
|
For generations, millions upon millions of babies were
routinely circumcised without anaesthetic, in the comforting
belief that "babies can't feel pain" - and in spite of
those babies turning blue in the face trying to tell us they
can.
|
Once [the Gomco™ clamp] was carefully and correctly
in place, I started turning the clamp handle. I had
been told that newborns didn't feel pain which I
scarcely believed, when all of a sudden came screams
which loosened the paint on the wall.
What an eye-opening, eardrum damaging event. I had
heard and seen battle injured soldiers before but this
screaming raised the hair on my neck.
- Dr.
Phillip Leveque
|
|
I am an American white female age 56, and I worked in
many family practice doctor's offices over the years.
Part of my job was to assist with circumcisions. I
quit my job over that very duty. It was barbaric. I
watched babies pass out, turn blue, scream in a
guttural scream that turned my blood cold. Parents
should be forced to watch a doctor cut off the tip of
their son's penis, hear him scream, see his skin
mottle white and blue, watch his head roll back and
forth in agony while strapped down, unable to move.
Babies have no voice in the decision other than
vomiting all over themselves during the "procedure".
If parents want that for their son, they should be
forced to participate in the torture.
Zuzu on Chron.com, May 19, 2011
|
|
Noah was circumcised yesterday (no bashing please,
this was our choice) and it was very traumatic,
probably more for me than for him. [She
wishes.] I did stay in the room with
him while they did it and did my best to comfort him
and give him his sugar binky. They
kept telling me that usually the babies will sleep
through the procedure. Noah didn't, he SCREAMED the
entire time. I was brought to tears, I hate
seeing my son so upset. Now he is screaming each time
I change his diaper. There's minimal bleeding, but his
penis is pretty swollen. I've been giving him
ibuprofen every 6 hours, but he still seems to be in
quite a bit of pain with each diaper change. It is so
hard for me to change him, and get his penis cleaned
while he is screaming like that (I am doing it, I just
don't like it). I don't know what else I can do to
comfort him. ...
- athiede on Cafemom, December 15, 2011
reply by mommy2brandon11: ...
I give you a lot of credit for being in
the room while they did the procedure I was not and I
do not think that I could have been either.
reply by mommyal060911: Me too! That is very brave. I
refused. My husband was in the room with our first
son, but he said he couldn't handle going in there
again with our second son.
[Raising the question, if they
couldn't bear to stay there, why did their babies
have to?]
|
(offsite) Dawn tells what happened after the doctor told her "he wouldn't feel a thing",
with photographs, in Everything Birth, April 27, 2013
Babies feel pain...
|
"Infants have the same capacity for pain as adults.
...By 20 weeks' gestation, ascending fibers,
neurotransmitters, and the cerebral cortex are
developed and function to the extent that the fetus is
capable of feeling pain. ...However, inhibitory
neurotransmitters are in insufficient supply until
birth at full term.
Preverbal [not yet speaking] infants are at high risk
for undertreatment of pain because of persistent myths
and beliefs that infants do not remember pain.
Therefore the preterm infant is rendered more
sensitive to painful stimuli. ...New research
indicates that repetitive and poorly controlled pain
in infants can result in lifelong adverse consequences
such a neurodevelopmental problems, poor weight gain,
learning disabilities, psychiatric disorders and
alcoholism (Anand, 2000)" (Jarvis, 2004, p. 211).
Jarvis, C. (2004). Physical examination & health
assessment (4th ed.). St. Louis, MO: Elsevier. Anand,
KJS: Effects of perinatal pain and stress, Prog Brain
Res 122:117-119, 2000. Anand, KJS: The applied
physiology of pain. In Anand KJS, McGrath, RJ,
editors: Pain in neonates, Amsterdan, 1993, Elsevier.
|
Porter et al. guessed that circumcision would be painful, and
surprise! It was.
|
Procedural Pain in Newborn
Infants: The Influence of Intensity and
Development
Fran Lang Porter, PhD, Cynthia M. Wolf, PhD, and J.
Philip Miller, AB
"We had hypothesized that circumcision would be at
the most invasive end of the spectrum, and this
procedure did elicit the most vigorous physiologic
and behavioral reactions of those we studied.
Similarly, clinicians rated circumcision as the most
painful of 12 clinical procedures. Thus, there was
convergence in a hypothetical gradient of pain, a
survey-based gradient of pain, and the infants'
actual responses to one procedure, circumcision."
PEDIATRICS
Vol. 104 No. 1 July 1999, p. e13.
|
That circumcision is acutely painful was scientifically
demonstrated in 1994:
| ACETAMINOPHEN ANALGESIA IN NEONATAL CIRCUMCISION:
THE EFFECT ON PAIN
Cynthia R. Howard, MD; Fred M. Howard, MD; and
Michael L. Weitzman, MD, Pediatrics, April 1994
Objective. Recognizing the concerns about the use of
local anesthesia in neonatal circumcision, a painful
procedure usually performed without analgesia or
anesthesia, we undertook a study of acetaminophen for
pain management of this procedure.
Design. A prospective, randomized, double blind,
placebo-controlled, clinical trial of acetaminophen
analgesia in 44 healthy full term neonates undergoing
circumcision was conducted. Beginning two hours before
Gomco circumcision, neonates received either
acetaminophen (15 mg/kg per dose, 0.15 mL/kg per dose)
or placebo (0.15 mL/kg per dose) every six hours for
24 hours. [There was no
control group left intact, who would of course
have experienced no pain.] Neonates
were monitored intraoperatively for changes in heart
rate, respiratory rate, and crying time. Postoperative
pain was assessed at 30, 60, 90, 120, 360 minutes and
24 hours using a standardized postoperative comfort
scoring system. Feeding behavior was also assessed
before and after circumcision by nursing observation.
Results. Neonates in both groups showed significant
increases in heart rate, respiratory rate, and crying
during circumcision with no clinically significant
differences between the groups. Postoperative comfort
scores showed no significant differences between the
groups until the 360-minute postoperative assessment,
at which time the acetaminophen group had
significantly improved scores. (P<.05). Feeding
behavior deteriorated in breast- and bottle-fed
infants in both groups, and acetaminophen did not seem
to influence this deterioration.
Conclusions. This study confirms that circumcision of
the newborn causes severe and persistent pain.
Acetaminophen was not found to ameliorate either the
intra-operative or the immediate postoperative pain of
circumcision, although it seems that it may provide
some benefit after the postoperative period.
Pediatrics 1994;93:641-646; neonatal circumcision,
acetaminophen.
... In summary, this study confirmed that circumcision
of the newborn causes severe and persistent pain.
Acetaminophen was not found to ameliorate the the
intraoperative or the immediate postoperative pain of
circumcision, although it may provide some benefit
after the immediate postoperative period. Given
the large numbers of newborns who undergo this
painful surgical procedure [This
is not a given. Parents could stop asking
for circumcision. Doctors could refuse to
circumcise. Pain is one of many reasons.],
it is imperative that safe and easily administered
methods of anesthesia be found and utilized.
Studies
like these raise serious ethical issues.
Experimentation on children is normally governed by
rigorous rules. Painful experimentation is
especially restricted. Only when it involves
circumcision, it seems, may doctors inflict major
pain on neonates with impunity.
|
Now the authorities are moving to "recommend" that anaesthetics
be used - but without ever admitting they were wrong to
circumcise all those babies without anaesthetic, and without
ever doubting the wisdom of circumcising at all.
Lander et al. found the
pain of circumcising without anaesthetic to be severe. The
circumcising of a control group without anaesthetic seems to
have been called off for ethical reasons. (There was no control
group of babies left intact.)
|
JOURNAL OF THE AMERICAN MEDICAL ASSOCIATION,
Volume 278 No. 24,
Pages 2157-2162,
December 24/31, 1997.
Comparison of Ring Block, Dorsal
Penile
Nerve Block, and Topical Anesthesia
for Neonatal Circumcision
A Randomized Controlled Trial
Janice Lander, PhD; Barbara Brady-Freyer, MN; James
B. Metcalfe, MD, FRCSC; Shermin Nazerali, MPharm;
Sarah Muttit, MD, FRCPC.
Abstract
Context. - Beliefs about the safety and
effectiveness of current anesthetics have resulted in
many newborns being circumcised without the benefit of
anesthesia.
Objective. - To compare ring block, dorsal
penile nerve block, a topical eutectic mixture of
local anesthetics (EMLA), and topical placebo when
used for neonatal circumcision. The placebo
represented current practice, with no anesthetic for
neonatal circumcision.
Design. - A randomized controlled trial.
Setting. - Antenatal units in 2 tertiary care
hospitals in Edmonton, Alberta.
Participants. [Participants
participate voluntarily. Those who do not are
called "subjects" or "victims".]. - A
consecutive sample of 52 healthy, full-term male
newborns, aged 1 to 3 days.
Interventions. - Physiological and behavioral
monitoring occurred in a series of trials: baseline,
drug application, preparation, circumcision, and
postcircumcision. Surgical procedures defined the
following 4 stages of the circumcision: cleansing,
separation, clamp on, and clamp off. Methemoglobin
level was assessed 6 hours after surgery.
Main Outcome Measures. - Heart rate, cry, and
methemoglobin level.
Results. - Newborns in the untreated placebo
group [that is, the
unanaesthetised, circumcised group. There was no
untreated control group] exhibited
homogeneous responses that consisted of sustained
elevation of heart rate and high pitched cry
throughout the circumcision and following. Two
newborns in the placebo group became ill following
circumcision (choking and apnea [i.e.they stopped breathing]).
The 3 treatment groups all had significantly less
crying and lower heart rates during and following
circumcision compared with the treated group. The ring
block was equally effective through all stages of the
circumcision, whereas the dorsal penile nerve block
and EMLA were not effective during foreskin separation
and incision. Methemoglobin levels were highest in the
EMLA group, although no newborn required treatment.
Conclusions. - The most effective anesthetic
is the ring block; EMLA is the least effective. It is
our recommendation that an anesthetic should be
administered to newborns prior to undergoing
circumcision.
[Not only would an
uncircumcised control group have demonstrated no
pain reactions, it would have provided valuable
baseline data. It seems the option of leaving any
babies uncircumcised was deliberately avoided.
Why?]
JAMA 1997; 278:
2157-2161
Part of the main text:
RESULTS
Part way through the trial, physicians and members
of the research team remarked that there were obvious
differences in behavior of newborns in either
infiltration group compared with those in both topical
groups. This led us to reexamine our estimation of
effect size as well as the ethical matters related to
sample size. [This has
commonly been interpreted to mean the experiment
was called off, but it may mean only that one baby
was withdrawn.]
[...]
Adverse Outcomes
A serious postsurgery incident was observed in 1
newborn in the placebo group. There was nothing
remarkable about this newborn's history prior to the
circumcision. His 1- and 5-minute Apgar scores were 9
and 10. He was last fed 3 hours before circumcision.
During and following circumcision, the newborn reacted
much the same as others who received a placebo
(continuously elevated heart rate and high-pitched
cry). About 2.5 minutes after the conclusion of
surgery, the new-born had an episode that included
abnormal posture (lack of tone in limbs), several
periods of apnea [not
breathing] (one lasting more than 25
seconds), and projectile vomiting. No physiological
data were recorded during the episode, since the
computer had lost contact with the monitor immediately
prior to its onset. The newborn recovered following
the episode.
Another newborn in the placebo group had a choking
episode with apnea after surgery. This began about 3.5
minutes after the circumcision and lasted less than 30
seconds.
[That's two serious adverse
outcomes out of only 12 babies circumcised without
anaesthetic, or 52 babies in the whole experiment.]
|
This study was videotaped, and the videotapes of the
unanaesthetised control group were extensively analysed. This
analysis is on another page.
In 2006 a baby died after his circumcision, and in response to
a complaint the doctor gave reasons he
still does not use anaesthesia.
Williamson and Evans found that, contrary to a common claim,
circumcision hurts much more than a heelstick, and local
anaesthetic is ineffective.
|
Clinical
Pediatrics August 1986 vol. 25 no. 8 412-415
Neonatal Cortisol Response to Circumcision with
Anesthesia
Paul S. Williamson, Nolan Donovan Evans
[Paul Williamson was a
co-author of the much-cited Iowa study that claimed to show women
prefer circumcised men. One of its subjects
has since written how it
was skewed.]
Abstract
Eleven male newborns were circumcised with a local
dorsal penile nerve block, and 13
controls were circumcised without anesthetic.
[How was this ethical, even in
1986?] Matched pairs of pre- and
postcircumcision cortisol levels in the two groups
were compared. The adrenal cortisol response to
surgery was not significantly reduced by the
administration of lidocaine. Blood
sampling and anesthetic injection of venipuncture
alone did not evoke the adrenal response in
uncircumcised control infants. Cortical input
or secondary epinephrine elevation may be producing
the cortisol elevation in infants despite regional
blockage of the afferent nerve pathways.
|
Slater et al. found that sugar-water is ineffective in
pain relief.
|
The
Lancet, Early Online Publication, 1 September 2010
Oral sucrose as an analgesic drug for procedural
pain in newborn infants: a randomised controlled
trial
Dr Rebeccah Slater PhD, Laura Cornelissen MSci,
Lorenzo Fabrizi PhD, Debbie Patten BSc, Jan Yoxen BSc,
Alan Worley MSc, Stewart Boyd MD, Judith Meek MBBS,
Prof Maria Fitzgerald PhD
Summary
Background
Many infants admitted to hospital undergo repeated
invasive procedures. Oral sucrose is frequently given
to relieve procedural pain in neonates on the basis of
its effect on behavioural and physiological pain
scores. [It is also commonly
given to babies undergoing ritual circumcision,
and sometimes to babies undergoing "medical"
circumcison.] We assessed whether
sucrose administration reduces pain-specific brain and
spinal cord activity after an acute noxious procedure
in newborn infants.
Methods
In this double-blind, randomised controlled trial, 59
newborn infants at University College Hospital
(London, UK) were randomly assigned to receive 0·5 mL
24% sucrose solution or 0·5 mL sterile water 2 min
before undergoing a clinically required heel lance.
Randomisation was by a computer-generated
randomisation code, and researchers, clinicians,
participants, and parents were masked to the identity
of the solutions. The primary outcome was
pain-specific brain activity evoked by one time-locked
heel lance, recorded with electroencephalography and
identified by principal component analysis. Secondary
measures were baseline behavioural and physiological
measures, observational pain scores (PIPP), and spinal
nociceptive reflex withdrawal activity. Data were
analysed per protocol. This study is registered,
number ISRCTN78390996.
Findings
29 infants were assigned to receive sucrose and 30 to
sterilised water; 20 and 24 infants, respectively,
were included in the analysis of the primary outcome
measure. Nociceptive [indicative of pain] brain
activity after the noxious heel lance did
not differ significantly between infants who
received sucrose and those who received sterile
water (sucrose: mean 0·10, 95% CI 0·04—0·16;
sterile water: mean 0·08, 0·04—0·12; p=0·46). No
significant difference was recorded between the
sucrose and sterile water groups in the
magnitude or latency of the spinal nociceptive reflex
withdrawal recorded from the biceps femoris of the
stimulated leg. The PIPP score was significantly lower
in infants given sucrose than in those given sterile
water (mean 5·8, 95% CI 3·7—7·8 vs 8·5, 7·3—9·8;
p=0·02) and significantly more infants had no change
in facial expression after sucrose administration
(seven of 20 [35%] vs none of 24; p<0·0001).
Interpretation
Our data suggest that oral
sucrose does not significantly affect
activity in neonatal brain or spinal cord nociceptive
[pain-receptive] circuits, and therefore might
not be an effective analgesic drug. The
ability of sucrose to reduce clinical observational
scores after noxious events in newborn infants should
not be interpreted as pain relief.
|
"It's over in a few seconds..." "...when performed by an
experience operator..."
Tauesch found that even with anaesthetic, pain was "excessive"
in three babies out of ten, and that the most experienced
operators could severely damage the penis.
|
Journal of Perinatology,
April/May 2002, Volume 22, Number 3, Pages 214-218
Pain During Mogen or PlastiBell Circumcision
H William Taeusch MD, Alma M Martinez MD, J Colin
Partridge MD, Susan Sniderman MD, Jennifer
Armstrong-Wells MD and Elena Fuentes-Afflick MD
...
This study was catalyzed by our
hospital's obstetric service choice not to carry out
circumcisions because of their belief that it
was medically unjustified.8
Pediatric staff decided to continue to provide
circumcisions gratis (MediCal does not reimburse
physicians for routine neonatal circumcisions) for
those parents who requested it, because we assumed
that the inconvenience, costs, and discomfort would be
greater if the procedure were carried out after the
newborn period.
...
Although circumcision is usually a rapid procedure in
the hands of skilled operators,13 no
studies have compared the amount of time required by
trainees to perform different techniques.
METHODS
The sample included term male infants born at San
Francisco General Hospital.
...
The infants' responses to the application of the first
foreskin clamp were graded by cry, with 0 to 1
indicating no or minimal response, 4 indicating a
lusty bellow of rage, and 2 and 3 indicating midrange
responses. This response was used to judge the
adequacy of the dorsal nerve block. Thereafter, infant
behaviors were graded using a scale of 1 to 7 that was
adapted and simplified from other neonatal pain
scores.18 A single grade, representing the
average behavior, was assigned for each 3-minute
period. Grade 1 was deep sleep indicated by regular
breathing, eyes closed, and no eye or extremity
movements. Grade 2 was rapid eye movement sleep
defined by rapid eyelid movements, irregular
respirations, and frequent limb movements or twitches.
Grade 3, a drowsy state, was characterized by eyes
mostly open and sparse body movements with some
sucking. An infant who was awake and alert, with eyes
occasionally fixing on objects, arms and legs moving,
no cry, some sucking movements, was assigned grade 4.
Grade 5 was defined by the infant
being fussy with infrequent soft vocalizations,
purposeful extremity movements against restraints,
active head motion, and a facial expression of
discontent. Grade 6 was scored for mild or moderate
crying. Grade 7 was defined by continuous loud
crying indicative of rage. The beginning of
the circumcision was recorded as the time the first
clamp was placed on the foreskin. The end of the
procedure was recorded when sterile drapes were
removed.
...
RESULTS
Sixty-one infants were enrolled in this study over a
2-year period from 1997 to 1998. Two were eliminated,
one for insufficient data and one for unclear
identification of the procedure, leaving 30 in the
Mogen group and 29 in the PlastiBell group included in
the analysis. The time from dorsal nerve block to
placing the first clamp on the foreskin was 6 minutes
for the group assigned to Mogen and 5 minutes for the
group assigned to PlastiBell (p>>0.05). No
difference in the response to placement of the first
clamp was found between the two groups (an average
score of 1 for each group). The efficacy of the dorsal
nerve block for all infants in the study is shown in
Figure 1, with approximately 65% of the infants having
a minimal (or no) response.
Figure 2 indicates that distribution of the duration
for the two techniques differs. Average
duration for the PlastiBell technique was 20±1.7
minutes (mean±SEM), and average duration for
the Mogen technique was 12±0.9
(p<0.001). Average pain scores over 3-minute
periods were identical in the two groups. They
averaged between 4 and 6 (Figure 3). Overall pain was
also scored for the entire procedure. Sixty
one percent of the entire sample had overall pain
scores of >4 with no differences between
groups. We did not assess
postoperative pain in this study.
We assessed the duration of the circumcision by level
of training of the operator. ...
On nine occasions for the Mogen
and seven for the PlastiBell, the procedure was the
first circumcision performed by the trainee.
No major complications were encountered by either
method during the course of the study (see Discussion
section for a complication incurred after the study).
In three instances, only the outer epidermal layer of
the foreskin was removed by the Mogen, leaving the
inner foreskin layer adherent to the glans. In these
cases, the inner foreskin layer was removed from the
glans and the time involved was included for the
duration of the original procedure. Informal reports
from our follow-up clinic indicated that mothers
occasionally complained that their infant did not
appear as if they had been circumcised (Mogen
technique), and two of these infants had a repeat
circumcision. We also received occasional complaints
from the outpatient clinic regarding the PlastiBell
technique. Issues included partial
separation of the plastic ring from the penis,
irregular foreskin removal, or swelling of the shaft
of the penis.
DISCUSSION
Circumcisions using the Mogen procedure were carried
out in about 60% of the time required for PlastiBell
circumcisions and because our measure of pain per time
period was similar for the two procedures, we assume
the overall pain of the Mogen procedure was less.
Probably because of our use of dorsal nerve blocks in
both groups, we found no difference in degree of pain
between procedures in the first 15 minutes, that is to
say, pain was related only to the efficacy of the
dorsal nerve block and to the duration of the
procedure. Total pain, however, is the product of
amount of pain times duration and more
than half of the study group had what we
considered excessive pain/discomfort over the
course of the entire procedure. We
agree with those who attribute much of the evident
discomfort (when dorsal nerve block is used
effectively) to the spread-eagled restraint of
extremities in extension on an unforgiving surface.
...
Two circumcisions were repeated after discharge of
the infant from the nursery, both after Mogen
procedures, and the amount of pain incurred in the
second circumcision is in addition to that of the
first. Removal of too small amount of foreskin such
that the infant looks uncircumcised was due to the
fear of amputation of the glans if more was removed.
In fact after completion of this study, approximately
10% of the glans of a newborn was amputated (it was
reattached surgically) during a Mogen circumcision carried
out by two of our most experienced physicians.
The cause was a small adhesion near the meatus that
was not lysed so that the glans was partially pulled
through the Mogen clamp and removed with the
foreskin. We have since modified the Mogen
procedure, still in use in our nursery, by carrying
out a dorsal slit of the foreskin and retracting it
fully to ascertain that no adhesions remain before
pulling it into the Mogen clamp for removal. This
modification has also been associated with no further
need for repeat circumcisions in over 200 Mogen
procedures done since the modification was put in
place.
Limitations of this study are several. Obviously the
study was not double-blind. ...
Behavioral testing for the assessment of pain, the use
of pain scores, has been cogently critiqued.20 ...
We did not assess the esthetics
of the results of the procedure or parent
satisfaction. [Or,
of course, patient satisfaction, when he
grows up.] Our sample was too small to
assess the relative safety of these techniques.
Advocates of circumcision and those against this
procedure both mount cogent arguments to support their
respective viewpoints.21,22,23 We believe more studies of the risk and benefits
of circumcision are needed. Outcome measures
should include acute and long-term adverse effects
like cosmesis, parent satisfaction, safety,
complications, long-term medical outcomes, and
ultimately an assessment of the feelings of the
circumcised or uncircumcised boy/adult, and possibly
his sexual partner(s).24,25,26 Sample sizes
in the thousands would be necessary and the cost of
the study would be high. However, current annual costs
of routine neonatal circumcision are ca. $150,000,000,
(est. 1,000,000 males in U.S. circumcised at $150
hospital+physician costs). Problems associated with
the uncircumcised state (increased risk of urinary
tract infections, sexually transmitted infections, and
phimosis, for example) are more difficult to estimate,
but may not be insignificant.1,21 Complications
of circumcision are probably underreported....
|
A 2005 study in Australia indicates that babies
feel pain more than adults.
So did a 2009 study in London:
|
Wellcome Trust
2 April, 2009
Feature: The pains of youth
By Mun-Keat Looi
As recently as the late 1980s, clinicians mistakenly
believed that newborn babies did not feel pain. We are
now beginning to understand just how different pain
processing is in infants, progress that promises
tremendous clinical benefits for those in intensive
care.
...
"Largely it was based on ignorance - a rather
simplistic view that if you can't remember something
then that means that you don't process it," says Maria
Fitzgerald, Professor of Developmental Neurobiology at
University College London.
...
Our pain pathways undergo extensive structural and
functional change after we are born. At first, the
nervous system is not fine-tuned, with nerve cells
underdeveloped and connections and circuits still raw.
"In very young babies there is a very strong,
exaggerated, behavioural response to pain, much
stronger than you would see in an older child or
adult," says Professor Fitzgerald.
Her latest research, funded by the Wellcome Trust,
has revealed a fundamental difference between infant
and adult pain pathways.
As adults, when we detect a painful stimulus, the
sensory nervous system in the spinal cord suppresses
the signal to a certain extent, reducing the intensity
of the pain and helping us to detect exactly where it
is in the body. Also, when the brain receives the pain
signal, it sends inhibitory information back to the
spinal cord.
But in newborn babies, this system has the opposite
effect.
"The brain actually enhances the pain inputs rather
than suppressing them. It's a complete reverse of what
happens in an adult," says Professor Fitzgerald.
...
Children that have undergone a lot of intensive care
when young seem to be less sensitive to things such as
touch and temperature. But they are more sensitive to
new pain stimuli. "It's quite an odd and complicated
picture, almost like a contrast. The child is
relatively less sensitive in its body but
hypersensitive, it seems, to a new pain," says
Professor Fitzgerald.
...
"There's
something about having an injury very early in life
that does seem to produce a very long-lasting
sensitivity in that injured area."
...
|
Taddio et al. found the
effects of the pain of circumcision could be detected months
later:
|
Abstracts - March 18, 1997 LANCET
Effect of Neonatal
Circumcision on Pain Response During Subsequent
Routine Vaccination
Background: Preliminary
studies suggested that pain experienced by infants in
the neonatal period may have long-lasting effects on
future infant behaviour. The objectives of this study
were to find out whether neonatal circumcision altered
pain response at 4-month or 6-month vaccination
compared with the response in uncircumcised infants,
and whether pretreatment of circumcision pain with
lidocaine-prilocaine cream (Emla) affects the
subsequent vaccination response.
Methods: We used a prospective cohort design
to study 87 infants. The infants formed three groups -
uncircumcised infants, and infants who had been
randomly assigned Emla or placebo in a previous
clinical trial to assess the efficacy of Emla cream as
pretreatment for pain in neonatal circumcision.
Infants were videotaped during vaccination done at the
primary care physician's clinic. Videotapes were
scored without knowledge of circumcision or treatment
status by a research assistant who had been trained to
measure infant facial action, cry duration, and visual
analogue scale pain scores.
Findings: Birth characteristics and infant
characteristics at the time of vaccination, including
age and temperament scores, did not differ
significantly among groups. [...]
infants circumcised with placebo had higher difference
scores than uncircumcised infants for percentage
facial action (136.9 vs 77.5%), percentage cry
duration (53.8 vs 24.7%), and visual analogue scale
pain scores (5.1 vs 3.1 cm). There was a significant
linear trend on all outcome measures, showing
increasing pain scores from uncircumcised infants, to
those circumcised with Emla, to those circumcised with
placebo.
[So anaesthesia does not
eliminate pain.]
Interpretation: Circumcised infants showed a
stronger pain response to subsequent routine
vaccination than uncircumcised infants. [No
good long-term studies have been done, but it
seems reasonable to conclude that some
physiological effects of circumcision may in fact
be life-long.] Among the circumcised
group, preoperative treatment with Emla attenuated the
pain response to vaccination. We recommend treatment
to prevent neonatal circumcision pain.
[But the paper has just
demonstrated that it doesn't prevent it.
Not circumcising would.]
(Lancet. 1997;349:599-603)
|
In 2002, Taddio et al.
found by comparing 21 babies of diabetic mothers (who underwent
repeated heelstick blood sampling) with 21 controls, that babies
learn to anticipate a painful stimulus by crying and
grimacing. In other words, they experience pain as pain,
consciously, not just as some kind of reflex.
|
Best Practice & Research Clinical
Anaesthesiology
Vol. 18, No. 2, pp. 357–375, 2004
available online at http://www.sciencedirect.com
Regional
anaesthetic techniques for neonatal surgery:
indications and selection of techniques
Martin Jöhr MD
Thomas
M. Berger MD
CIRCUMCISION
Clinical relevance
In some societies circumcision is performed in
virtually all boys at a very early age for
traditional or religious reasons. Other societies
perform this type of surgery only for medical
indications, such as phimosis or recurrent
infections. In the past, circumcision for
traditional or religious reasons has often been done
in awake neonates with minimal or even no pain
relief at all. [And in the
US, it still is.] Forceful
immobilisation, e.g. on a circumcision board, and
performance of the procedure in a crying patient has
been an accepted practice until recently. Today,
some type of procedural pain relief appears to be
mandatory for most practitioners.39 In Western
Europe, where circumcisions are largely performed
for medical indications, a major regional block with
a completely comfortable patient or a general
anaesthetic is mandatory. Performing
surgery on a crying patient would not be an
acceptable standard. These two completely
different attitudes might explain why for some
colleagues topical anaesthesia40 – 42 or oral
sucrose alone43,44 seem to be useful for procedural
analgesia during circumcision,45 whereas for others,
these techniques are clearly insufficient.
Penile
block
Dorsal nerve penile block had already been proposed
for neonatal circumcision by the late 1970s.46
Penile block, in Europe often combined with a
general anaesthetic, provides prolonged pain relief
for up to 6–24 h after penile surgery, much longer
than a caudal block [but
not nearly as long as the duration of pain from
urine in the wound, which takes at least a week
to heal.]. Two paramedian injections
of 0.1 ml/kg ...
Penile block has a good safety record: in a series
of 3909 penile blocks no permanent damage
occurred52, while inadvertent injection of the wrong
solution and urethral puncture during ring block
were the important and clearly avoidable
complications.
Caudal
or spinal anaesthesia
Single shot caudal anaesthesia can be used for
neonatal circumcision. In our practice, 3 ml of a
mixture at equal parts of lidocaine 1% with
bupivacaine 0.25% with epinephrine were clinically
effective in virtually all cases and had,
apparently, the advantages of relatively rapid onset
and prolonged pain relief. Nevertheless,
the role of neuraxial anaesthesia for this type of
intervention has to be questioned.
|
In February 2000, the American Academy of Pediatrics and the
Candian Paediatric Society issued a joint report
on neonatal pain. Eight of the references in this report
have "circumcision" in their titles, yet the report itself
mentions circumcision only once, and the pain of the actual
operation - surely the commonest and most severe pain
experienced by neonates in the US today - not at all.
|
Pediatrics
|
Volume 105, Number 2
|
February 2000, pp 454-461
|
|
|
Prevention and
Management of Pain and Stress in the Neonate
(RE9945)
AMERICAN ACADEMY OF PEDIATRICS
Committee on Fetus and Newborn
Committee on Drugs
Section on Anesthesiology
Section on Surgery
CANADIAN PAEDIATRIC SOCIETY
Fetus and Newborn Committee
ABSTRACT. This statement is intended for health care
professionals caring for neonates (preterm to 1 month
of age). The objectives of this statement are to:
- Increase awareness that neonates
experience pain;
[...]
- Make recommendations for reduced
exposure of the neonate to noxious stimuli
and to minimize associated adverse outcomes[...]
Studies indicate a lack of awareness among
health care professionals of pain perception,
assessment, and management in neonates.
[...]
Exposure to prolonged or severe pain may
increase neonatal morbidity.
Infants who have experienced pain during the neonatal
period respond differently to
subsequent painful events.
[...]
Neonates are not easily
comforted when analgesia is needed.
A lack of behavioral responses
(including crying and movement) does not
necessarily indicate a lack of pain.
GENERAL PRINCIPLES
[...]
Some studies suggest that pain experienced early in
life by term infants may
exaggerate affective and behavioral responses
during subsequent painful events.
[...]
Pain is managed most effectively by preventing,
limiting, or avoiding noxious stimuli [such as...]
and providing analgesia.13
[...]
PREVENTION OF ACUTE PAIN DURING OR AFTER SURGERY OR
A PAINFUL PROCEDURE
[...]
Nonsteroidal Anti-inflammatory Drugs
Generally, this category of medications is used to
treat less intense pain and as an adjunct to reduce the
total dose of more potent analgesics, such as opioids.
Limited data are available on the pharmacokinetics of
acetaminophen (paracetamol) in newborns. Acetaminophen
does not reduce the response to pain due to heel-lance
procedures but may provide some
reduction in pain after circumcision.
[Paracetamol! And this is the
only mention of circumcision in the whole paper. If
paracetamol doesn't reduce the pain of heel-stick,
why should it reduce the much greater pain of
circumcision?]
[...]
RECOMMENDATIONS
Health care professionals should use appropriate
environmental, nonpharmacological (behavioral), and
pharmacological interventions to prevent, reduce, or
eliminate the stress and pain of neonates.
[And the most appropriate
nonpharmacological, non-surgical (behavioural)
"intervention" to prevent, reduce, and (with total
certainty) eliminate the stress and pain of
circumcision is of course, not circumcising.]
|
Taddio et al. have published another pain study, with an
extraordinarily basic flaw:
|
Arch
Pediatr Adolesc Med 2000 Jun;154(6):620-3
Combined
analgesia and local anesthesia to minimize pain
during circumcision.
Taddio
A, Pollock N, Gilbert-MacLeod C, Ohlsson K, Koren
G
Department of Pharmacy, The Hospital for Sick
Children, Toronto, Ontario, Canada. anna.taddio@sickkids.on.ca
[Medline record in process]
BACKGROUND:
Pain of circumcision is only partially relieved by
single modalities, such as penile nerve block,
lidocaine-prilocaine cream, and sucrose pacifiers.
OBJECTIVE:
To assess the effectiveness of a combination of
interventions on the pain response of infants
undergoing circumcision.
METHODS:
Cohort study.
Group 1 included infants circumcised using the Mogen clamp and
combined analgesics (lidocaine dorsal penile nerve
block, lidocaine-prilocaine, acetaminophen, and
sugar-coated gauze dipped in grape juice).
Group 2 included infants circumcised using the Gomco clamp and
lidocaine-prilocaine. Infants were videotaped
during circumcision, and pain was assessed using
facial activity scores and percentage of time
spent crying.
RESULTS:
There were 57 infants in group 1 and 29 infants in
group 2. Birth characteristics did not differ
between groups. Infants in group 1 were older
than infants in group 2 (17
days vs 2 days)
(P < .001). The mean duration of the
procedure was 55 seconds
and 577 seconds for
infants in group 1 and 2, respectively
(P < .001). Facial action scores and
percentage of time spent crying were significantly
lower during circumcision for infants in group 1
(P < .001). The percentage of time
spent crying was 18% and 40% for infants in groups
1 and 2, respectively. No adverse effects were
observed in infants in group 1; 1 infant in group
2 had a local skin infection.
CONCLUSIONS:
Infants circumcised with the Mogen clamp and
combined analgesia have substantially less pain
than those circumcised with the Gomco clamp and
lidocaine-prilocaine cream. Because of the immense pain during
circumcision, combined local anesthesia and
analgesia using the Mogen clamp should be
considered.
[The conclusion patently
does not follow from the experiment:
- One group was much older than
the other
- One group was circumcised by a different
method from the other, and of those
- One method took 10 times as long
as the other
- One group was given different anaesthesia/analgesia
from the other
Any of these factors could be
responsible for the differing pain suffered by
the two groups.
Predictibly, the two groups were not
contrasted with a control group of babies left
intact. It is, of course, safe to predict that
such a group would experience no pain at all,
but it is as though these scientists don't
want to consider the option of leaving babies
alone.
The method they recommend, the Mogen clamp (a
slicing rather than crushing method), carries
a greater risk of trapping and slicing the
glans because it is a "blind" method, as Varney's
Midwifery points out.
Prilocaine - used in
both kinds of circumcision - is implicated in
methaemoglobinaemia, according to the British
Journal of Urology: Toxic neonatal
methaemoglobinaemia after prilocaine
administration for circumcision ]
PMID: 10850512, UI: 20306685
http://archpedi.ama-assn.org/issues/v154n6/full/poa90426.html
|
Ruda et al show that pain in neonates causes changes in
pain-sensitivity in adulthood.
|
From Science, July 2000
Once Bitten, Twice
Sensitive
Advances in operation techniques and other medical
treatments have improved the survival chances of
immature or otherwise medically compromised neonates.
Do such tissue damage and painful interventions early
in life have adverse long-term effects? Ruda et al.
... show that hindlimb inflammation in rat pups
triggers exuberant growth of small-diameter,
pain-transmitting axons in the dorsal horn of the
spinal cord. These changes are coupled with an
increase in the sensitivity of the paw after
inflammation in the adult. These results show that painful stimuli in early
development can cause long-term alterations in the
neuronal circuitry.
Ruda MA, Ling Q, Hohmann AG, et al. Altered
Nociceptive Neuronal Circuits After Neonatal
Peripheral Inflammation. Science 2000; July 28 :
|
From
New Scientist
5 August 2000, p25
IN BRIEF
Painful
Start
OPERATING on fetuses and newborns might make them
more senstitive to pain later in life, say researchers
at the National Institutes of Health, near Washington
DC.
Mary Ann Ruda and colleagues simulated surgery on
newborn rats by injecting an inflammatory agent into a
hind paw. When the rats reached adulthood, they
withdrew the test paw from a hot bulb much faster than
rats that had been injected with saline as newborns
(Science, vol 289, p628). They also had more nerves in
the region.
Until the 1980s, anaesthesia was rarely given to
newborns because their nervous system was considered
immature. Even today, anaesthetics given to the mother
during fetal surgery do not reach the fetus, Ruda
says. "Now is a good time to find people who had
procedures as infants and test for differences in
their pain sensitivity."
[She won't have to look far!]
|
Murphy et al. found that early pain changes the
brain
|
Science Daily
Pain in Infancy Alters Response to Stress, Anxiety
Later in Life
Oct. 30, 2013 — Early life pain alters neural
circuits in the brain that regulate stress, suggesting
pain experienced by infants who often do not receive
analgesics while undergoing tests and treatment in
neonatal intensive care may permanently alter future
responses to anxiety, stress and pain in adulthood, a
research team led by Dr. Anne Murphy, associate
director of the Neuroscience Institute at Georgia
State University, has discovered.
An estimated 12 percent of live births in the U.S.
are considered premature, researchers said. These
infants often spend an average of 25 days in neonatal
intensive care, where they endure 10-to-18 painful and
inflammatory procedures each day, including insertion
of feeding tubes and intravenous lines, intubation and
repeated heel lance. Despite evidence that pain and
stress circuitry in the brain are established and
functional in preterm infants, about 65 percent of
these procedures are performed without benefit of
analgesia. Some clinical studies suggest early life
pain has an immediate and long-term impact on
responses to stress- and anxiety-provoking events.
The Georgia State study examined whether a single
painful inflammatory procedure performed on male and
female rat pups on the day of birth alters specific
brain receptors that affect behavioral sensitivity to
stress, anxiety and pain in adulthood. The findings
demonstrated that such an experience is associated
with site-specific changes in the brain that regulate
how the pups responded to stressful situations.
Alterations in how these receptors function have also
been associated with mood disorders.
The study findings mirror what is now being reported
clinically. Children who experienced unresolved pain
following birth show reduced responsiveness to pain
and stress.
"While a dampened response to painful and stressful
situations may seem advantageous at first, the ability
to respond appropriately to a potentially harmful
stimulus is necessary in the long term," Dr. Murphy
said.
"The fact that less than 35 percent of infants
undergoing painful and invasive procedures receive any
sort of pre- or post-operative pain relief needs to be
re-evaluated in order to reduce physical and mental
health complications associated with preterm birth."
The research team included scientists at Georgia
State's Center for Behavioral Neuroscience and Yerkes
National Primate Center. Results of the study were
published in the most recent edition of the journal
Psychoneuroendocrinology. The peer-reviewed journal
article summarizes research led by Murphy and graduate
student Nicole Victoria from Dr. Murphy's lab. Also
involved were Dr. Larry Young (Yerkes Division of
Behavioral Neuroscience & Psychiatric Disorders
and the Center for Translational Social Neuroscience)
and postdoctoral fellow Dr. Kiyoshi Inoue from the
Young lab.
The paper is:
Nicole C. Victoria, Kiyoshi Inoue, Larry J. Young,
Anne Z. Murphy
Long-term dysregulation of brain corticotrophin and
glucocorticoid receptors and stress reactivity by
single early-life pain experience in male and female
rats.
Psychoneuroendocrinology, 2013; DOI:
10.1016/j.psyneuen.2013.08.013
|
It has long been the speculation of these pages that
circumcision causes the nervous system to reinterpret the
signals from the pain-receptors of the glans in terms of pleasure,
using the genital pleasure centres of the brain left unemployed
by the removal of the foreskin. These experiments indicate a
complicating factor to that supposition. In any case, they throw
another spanner in the works of the idea that "babies can't feel
pain, or if they can, they soon forget it."
Persistent pain after adult circumcision
|
Q: Since a circumcision eight months ago I suffer
constant pain which is eased a bit by Pregabalin
tablets. My GP says my nerve ends may never heal,
but is there any other effective treatment of any
kind?
A: Any surgical scar has the potential to cause
persistent pain but it is a rare complication and the
causes are poorly understood. It is postulated that
the scar or the surgery interferes with the normal
function of the nerves that supply the area. Those
nerves would normally register normal sensations of
touch, temperature, pressure and pain. For some reason
the pain-sensing nerves behave abnormally and
constantly register pain for which there is no
apparent cause. It often has an unusual quality and is
referred to as “neuropathic pain”. Standard
painkillers are usually ineffective but a group of
drugs which alter nerve function can ameliorate the
pain to some degree. Pregabalin is one of these and it
is worth trying others in the group as individuals can
react differently to specific drugs. I have several
patients in whom the intensity of the pain has slowly
faded over a long period of time when medication can
then be withdrawn, others are not so fortunate. So
your pain may settle yet.
- Dr David Roche answering a query on Saga, March 29, 2012
|
Pain synaesthesia
An unusual condition, but a striking illustration:
New
Scientist
17 April 2010
Empathy
excess
From Jaques de Boys
Helen Thompson writes that all documented pain
synaesthetes suffered traumatic pain before developing
the condition: Many are amputees, and their phantom
limb is the site of the pain the feel when faced with
another's distress (13 March, p42)
All my life - I am now 64 - whenever I heard about
someone being sliced by a sharp object I felt a sharp
pain in my circumcision scar. Now I know why. My case
may expand the understanding of this phenomenon:
unlike most amputees, I was only a week old when I was
circumised and have no conscious memory of it.
It was a routine circumcision performed by a
competent doctor, but late in 1945 newborns being
circumcised in the UK probably did not receive any
anaesthetic.
Address supplied, Canada
|
Animals protected
Anesthesia is required by U.S. federal law for any painful
procedure on a veterinary or lab animal. See: 7 USC
54 Sec. 2143, which dates to the 1960’s. (A researcher was
dismissed from the University of Washington a few years ago for
operating on mice without it.)
No such law exists to protect children.
In Nigeria, where most babies are cut without
anaesthetic, this is considered ethical
Niger Med J. 2020 Jan-Feb; 61(1): 11–15.
Published online 2020 Mar 2. doi: 10.4103/nmj.NMJ_68_19
A Comparison of Pain Scores in Neonatal
Circumcision with or without Local Anesthesia in Jos,
Nigeria
Aminu Gango Fikin1 and Stephen Yohanna
Abstract
Introduction:
Neonatal circumcisions are commonly performed in
Nigeria, most often without anesthesia. The aim of this
study was to determine whether anesthesia was required
for neonatal circumcision.
Materials and Methods:
All new-born male neonates presenting [no,
being presented] for routine
circumcision were considered for inclusion in the study.
This was a randomized control study, comparing pain
scores during circumcision with local anesthesia or
without local anesthesia. A total of 72 neonates were
randomly assigned to the two groups using
computer-generated random numbers, with 36 in each
group. The neonates were not matched for age or weight.
All the anesthetic procedures and circumcisions were
performed in identical manner by the principal
investigators using the plastic bell technique. Approval
for the study was obtained from the Research Ethics
Committee of the hospital. Written voluntary informed
consent was obtained from the parents
of the neonates. [Were
they really told that there was a 50:50 chance that
their baby would be cut without anaesthetic?]
Results:
The mean age and weight of the neonates in the study
were 17 ± 2 days and 3.2 ± 0.68 kg, respectively. The
mean Neonatal/Infant pain score was 4.8 in the local
anesthesia group and 6.0 in those without anesthesia.
The mean transcutaneous PO2 was 90.47 ± 7.53 in those
with anesthesia compared to 85.83 ± 5.61 in those
without anesthesia. The mean heart rate was 133.88 ±
35.00 beats/min in the anesthesia group compared to
152.11 ± 79.80 in those without anesthesia. Neonates
circumcised without local anesthesia had higher
respiratory rate compared to those circumcised with
local anesthesia.
Conclusion:
Neonates circumcised without local anesthesia had higher mean pain scores, heart
rate, lower oxygen saturation and increased mean
respiratory rate than those that had local
anesthesia. Local anesthesia should be routinely used
during neonatal circumcision [or
babies' foreskins should not be cut off].
[As usual there was no
control group left intact, who can confidently be
predicted to have felt no pain at all.]
|
Related pages:
Back to the Intactivism index page.
|
|